Background
The combination of exposure to a risk and occurrence of the disease makes it more likely that an individual will be admitted to hospital. In a case-control study, this means the hospital cases could have higher risk exposures or disease than cases from the population at large. This can affect the estimates of the association between the exposure and the disease.
Admission bias is also known as Berkson’s bias (Berkson 1946). His original work involved a retrospective study examining disease risk factors from a hospital in-patient population. Berkson’s choice of inpatients resulted in a spurious association between the disease and the risk factors under study.
Example
Berkson described assessment of the relationship between gallbladder disease (as a possible cause) and diabetes. Because the study involved participants attending a clinic, whose attendance (overall) was affected both by gallbladder disease and by diabetes, this biased the association between gallbladder disease and diabetes. (Berkson 1946).
In a more recent example, researchers looked at blood pressure among people attending a hospital clinic with recurrent attacks of a migraine or headaches and found that the prevalence of high blood pressure was about 38% compared with the general population rate of 11%. They suggested those attending a hospital clinic are likely to have more associations between the two medical conditions than those present in the general population (Prudenzano et al. 2005).
Sackett (1979) tested for Berkson’s bias in interviews of random samples of the general population to determine the presence or absence of respiratory disease and locomotor disease. He then looked at the same thing for those within the sample who had been hospitalised in the previous six months. The results are in the table:
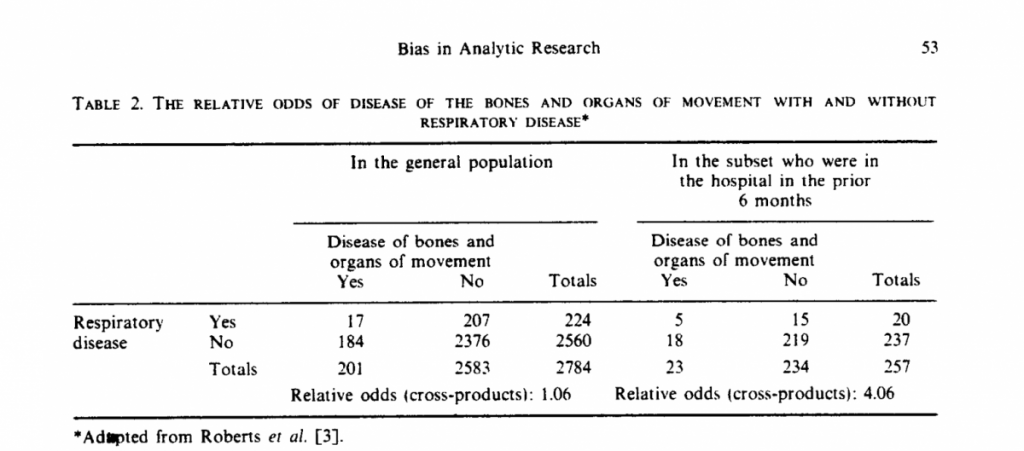
In the hospital sample, people with respiratory disease are much more likely to suffer from locomotor disease (Relative odds 4.06). We might conclude (incorrectly) there are associations between these two diseases.
If we looked at the general population, we would conclude there is no association between the two diseases (Relative odds 1.06) – the correct conclusion. The incorrect conclusion arises because people who have both disorders are more likely to be hospitalised.
Impact
Sackett’s 1979 paper points out that relative odds may be spuriously increased or reduced by the presence of admission rate bias.
There is evidence that having malaria increases your chances of suffering non-typhoidal salmonella infection. Researchers looking at this association suspected that Berkson’s bias would have an impact and that as a result, case-control studies of this association among patients in hospitals might give biased results.
The researchers did two case-control studies using two different methods of selecting controls (Krumkamp et al. 2016). In the first study, children with salmonella infection were classified as cases, and controls were uninfected. A protective association between malaria and salmonella infection was found: pooled OR = 0.4. In the second study, children testing positive for salmonella were cases, and children with another type of bacterial infection (not salmonella) were controls. In this study, malaria was a risk factor for salmonella infection: pooled OR = 1.9
In this example, both the “exposure” of malaria and the “outcome” of salmonella infection were factors that caused people to attend hospital, affecting the relationship between these two outcomes. Berkson’s bias caused the result to be reversed from one study to the other.
In another example, researchers looked at risk factors for bladder cancer, the risk of which is increased by smoking (Sadetzki 2003). Using a hospital-based case-control study design, they found very little association between smoking and bladder cancer; however, looking again, they noted that rates of smoking were much higher in their sample than in the general population, for both the cases and controls. This may have distorted the nature of the relationship between smoking and bladder cancer.
Preventive steps
Selection of appropriate controls for a case-control study is critical for obtaining the best possible information, and Berkson’s bias should be considered and plans made to avoid this wherever possible. In a study using data from hospitalised cases it might be preferable to use matching controls which are also in hospital, but using controls from the general population is better, to avoid Berkson’s bias.
Indirect Berkson’s bias (exposure-disease associations that arise because another disease is associated with the exposure under study) is attenuated mainly by using incident cases (i.e. not prevalent, already-existing cases). It can also be avoided by excluding patients who have been hospitalised because of another disease.
When an association between an exposure and an outcome is known to affect the selection of cases and controls into a study (e.g. in a hospital setting), it is preferable to adjust the analysis to try to deal with this bias.

